
| J EMMETROPIA VOLUME 3 NUMBER 3 | << BACK |
Q Factor Presbylasik.
Fundamentals and therapeutic approach
Fundamentals and therapeutic approach
Alfredo Amig� MD, PhD1; Sergio Bonaque-Gonz�lez, MSc1
ABSTRACT: The influence of spherical aberration (SA) on presbyopia symptoms is not sufficiently well known, although there is growing interest due to its potential applications during laser corneal surgery in patients with presbyopia. This update/review aims to describe and clarify the positive and negative effects of SA on presbyopia and its relation to corneal asphericity (Q factor) so that, by customizing it during surgery, symptoms can be improved.
J Emmetropia 2012; 3: 167-171
J Emmetropia 2012; 3: 167-171
1 Instituto Oftalmol�gico Amig�, Tenerife, Spain.
Financial disclosure: The authors state no financial disclosure with any of the contents of the manuscript.
Corresponding author: Alfredo Amig�. Instituto Oftalmol�gico Amig�, C/ El Humo 1-1oA, 38003 Tenerife, Spain.
E-mail: [email protected]
Financial disclosure: The authors state no financial disclosure with any of the contents of the manuscript.
Corresponding author: Alfredo Amig�. Instituto Oftalmol�gico Amig�, C/ El Humo 1-1oA, 38003 Tenerife, Spain.
E-mail: [email protected]
INTRODUCTION
The interest in improving presbyopia symptoms during corneal laser surgery has led to the proposal of innovative correction methods by means of corneal customised treatments. Special attention has been focused on the induction of spherical aberration (SA) by modifying the Q factor of the cornea1-3.
The aim of this article is to describe, in practical terms for the refractive surgeon, the influence of SA on presbyopia and the fundamentals for improving its symptoms during corneal correction with laser by modifying corneal asphericity.
Fundamentals of SA and its relation to presbyopia
In simplified terms, spherical aberration (SA) can be described as a high-order aberration caused by an unequal convergence of the central and peripheral rays passing through the refractive surfaces of the eye and striking parallel to the optical axis4. Total SA is defined as the sum of the SA of the anterior and posterior surfaces of the cornea and the lens-induced SA; the total SA will eventually affect the image formed on the retina and therefore, visual quality.
aberration caused by an unequal convergence of the central and peripheral rays passing through the refractive surfaces of the eye and striking parallel to the optical axis4. Total SA is defined as the sum of the SA of the anterior and posterior surfaces of the cornea and the lens-induced SA; the total SA will eventually affect the image formed on the retina and therefore, visual quality.
Two main types of SA are described. If in an optical system the peripheral rays from the object focus behind the plane where the central rays focus, it is said that the system has negative spherical aberration (-SA); when it is the other way around, it is said that it has positive spherical aberration (+SA)4.
Well-known examples are: the aberration induced by myopic corneal treatments which make the cornea more oblate, increasing +SA, and hyperopic treatments which make the cornea more prolate, increasing -SA5 (Figure 1).
The relationship between SA and refraction
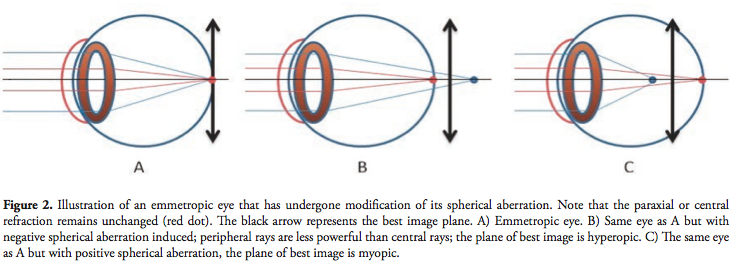
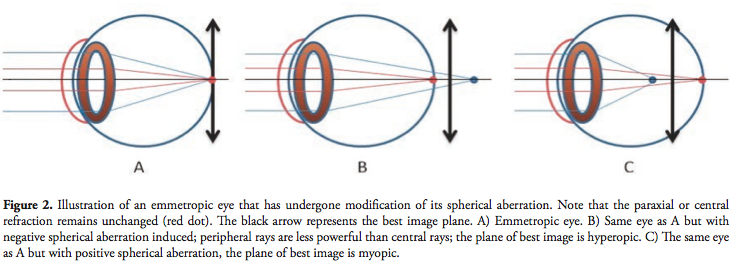
The interaction between SA and ocular refractive status is not a recent discovery. An attempt had already been made in 1944 to describe this phenomenon6, although it was not always well understood. We currently know that the presence of a spherical aberration in an optical system displaces the best image plane with regard to the plane where the paraxial rays are focused (the paraxial plane), in such a way that the induction of -SA will modify the ocular refractive status, making it more hyperopic; on the contrary, if +SA is induced, there will be myopic displacement.
Data of practical interest for refractive surgery can be obtained from these phenomena, and can be summarised as follows: if we obtain emmetropia in the presence of a certain amount of SA, as the latter decreases, the ocular refractive status (best image plane) will tend towards hyperopia; if this pre-existing SA increases, it will tend towards myopia (Figure 2).
To understand how these optical or refractive phenomena can affect presbyopia, we must first further explain the relationship between SA and pupil diameter, as it is one of the major modifying agents that affects SA-induced refractive change (Invest Ophthalmol Vis Sci 2006; 47: E-Abstract 5844). The influence of the pupil is obvious if we take into account that if we decrease the diameter of the pupil, the peripheral rays will gradually disappear until there is only one focus: the central one (very close to the paraxial one). Therefore, if an average eye presents SA, it will be highest with a wide pupil, and will gradually decrease until it practically disappears during pupil miosis, just as it does during physiologically-activated accommodative miosis in near vision7. (Figure 3)
as it is one of the major modifying agents that affects SA-induced refractive change (Invest Ophthalmol Vis Sci 2006; 47: E-Abstract 5844). The influence of the pupil is obvious if we take into account that if we decrease the diameter of the pupil, the peripheral rays will gradually disappear until there is only one focus: the central one (very close to the paraxial one). Therefore, if an average eye presents SA, it will be highest with a wide pupil, and will gradually decrease until it practically disappears during pupil miosis, just as it does during physiologically-activated accommodative miosis in near vision7. (Figure 3)
We can thus derive a first refractive aspect that is not yet fully disseminated among ophthalmologists. A patient with emmetropic refraction and significant positive SA, such as can be present after classic myopic lasik treatments, will really have a fluctuating refraction depending on the pupil diameter, so that when the pupil contracts during accommodative miosis, the disappearance of SA will cause a hyperopic shift in the refractive state of the eye (Figure 4) that must be compensated by accommodation (accommodative lag), exacerbating presbyopia symptoms, Postoperatively, this is usually identified by the ophthalmologist as an early presbyopia manifestation, when what really occurs is that an increase in +SA causes proportional worsening of symptoms3,8.
hyperopic shift in the refractive state of the eye (Figure 4) that must be compensated by accommodation (accommodative lag), exacerbating presbyopia symptoms, Postoperatively, this is usually identified by the ophthalmologist as an early presbyopia manifestation, when what really occurs is that an increase in +SA causes proportional worsening of symptoms3,8.
The contrary is true for negative SA. An emmetropic eye with -SA, such as we can find after total hyperopic ablation, will have myopic refraction during accommodative miosis (Figure 5), improving presbyopia symptoms3,8. Therefore, the presence of a certain degree of -SA can be beneficial for a patient with presbyopia. Presbyopic lasik (also known as "presbylasik") is based on this optical phenomenon, modifying the Q factor which, as we shall see, is ultimately based on the customised modification of the total SA.
Therapeutic approach by customised induction of SA
We can already describe an approach that allows us to treat presbyopic patients with corneal ablations, based on four points in the following order:

1.) Avoid inducing +SA. Even though new aspheric profiles in currently used laser platforms have decreased the amount of induced +SA, especially in moderate to high myopia, if no adequate preventive measures are taken, +SA is still significantly induced.
2.) Reduce pre-existing +SA. The human eye has a slightly positive mean total +SA, of the order of 0.12 µm9,10. This relatively small amount of SA may still induce a hyperopic shift during pupillary miosis (approx. 0.3 D) and must be corrected. This effect will be greater when dealing with higher preexisting +SA3.
3.) Induce -SA when necessary. By using an approach that has already been described2,3, we can induce a certain amount of net -SA to obtain a relative myopic shift during accommodative miosis, creating what has been called "accommodation by pupil miosis", that allows us to further improve the symptoms of presbyopia. Recent theoretical studies have shown that this effect can add approximately 0.7 D to the eye, assuming a wide pupillary range is present (6 to 2 mm)3. However, in order to achieve this, we must first avoid and/or remove all +SA.
4.) Add small amounts of monovision (micro-monovision). A certain amount of monovision may be more efficient and better tolerated in the presence of -SA11. This is true if we take into account that when reducing +SA, micro-monovision offers a complementary and significant addition that would otherwise be insufficient if +SA was present.
Relationship between SA and corneal asphericity (Q factor)
So, how can we reduce +SA and even induce a certain amount of -SA? One way to achieve this is by modifying the corneal asphericity.
Corneal asphericity refers to the difference between the central and peripheral radii of curvature12. This difference is expressed by means of different form factors such as the well known Q factor or eccentricity; its conversion factor is based on the formula (P = Q + 1=1=1�e2 =E�1)7.Tosimplify,wewillexpressit using the Q factor.
There is a close relationship between the Q factor and the induced SA such that as the Q factor becomes more negative, or the lower it is, the more the total SA decreases or becomes negative and vice versa13. The normal human cornea has a Q value of -0.26, corresponding to a certain amount of +SA14,15. In classic myopic laser treatment, the Q factor becomes more positive, inducing +SA15, which is exactly what we have to avoid; this can be achieved by modifying corneal asphericity during laser treatment. An increasing number of laser platforms currently allow the Q factor to be modified at the time of myopic or hyperopic treatment.

How much though do we have to modify this factor, and what are the limits of this modification? This is probably the most sensitive issue pertaining to this technique, as inducing an excessive -SA < -0.4 µm is not only ineffective3, but can also negatively affect the final visual quality16. Decreasing the Q factor to approximately -0.7 at 20o from the centre of the cornea is, in most cases, enough to free an average eye from any amount of significant pre-existing SA3, which in addition to not hindering visual quality, does not worsen presbyopia symptoms, allowing satisfactory near vision without correction in most patients until the age of 45. After this age, if we want to extend the effectiveness of the treatment to as many years as possible, we usually have to induce -SA, and therefore the Q factor must be decreased further than -0.7. This is a more complex field, as the final SA will depend on three major modifiers or preoperative variable factors: pre-existent total SA, Q factor and pupil range. As a rule, we can consider two potential scenarios in which we should not exceed the final target Q value of -1:
a) Patients with scotopic pupil diameter > 6 mm.
b)Patients with lower pre-existing physiological +SA, particularly in those uncommon, albeit possible, cases in which it is already negative.
Tables 1 and 2 show different surgical examples of how the Q target must be adjusted to avoid exceeding -0.4 µm of -SA, depending on the two major modifiers: preoperative total SA (Table 1) and the pre-existing corneal asphericity (Table 2).
Other variables or minor modifiers such as the magnitude of the ablation to be corrected (variation in the corneal radius) are barely clinically significant3. The third major modifier, pupil range, is probably the most important with regard to the decision of whether or not to modify the Q value. A wide pupil range, from 6 mm in meso-scotopic to 2 mm in accommodative miosis, will offer the greatest refractive benefit or accommodation by pupil miosis, thus achieving an extra addition for near vision, derived from the removal of pre-existing +SA and the induction of �SA.
On the other hand, patients with limited pupil ranges or with small pupils will not obtain a significant accomodative benefit from modifying the Q factor. As we have previously mentioned, the total SA practically disappears for pupil diameters smaller than 3 mm. (Figure 3)
Influence of the Q factor on the nomograms
We have mentioned the importance of customized modification of the Q factor in order to correct or induce SA. Nonetheless, this manipulation will give rise to a clinical problem due to the change in final refraction that systematically accompanies this modification hypercorrection in myopic ablations and hypocorrection in hyperopic ablations. For this reason, the nomogram must be customised for each laser platform. This modification is reasonably straightforward in those models that have software indicating the microns of ablation in each treatment, either standard or with modified Q factor. We can thus prevent hyperor hypocorrections by increasing or decreasing the spherical component to be corrected until the final ablation microns of the customised treatment match those of the standard treatment.
Quantifying anatomical results
Quantification of the anatomical results through corneal topography can be difficult to interpret.
Issues such as in which optical area the modification of the Q factor obtained should be assessed, and the variations existing between the different instruments make it advisable to study the results indirectly through measurement of total aberrometry. Thus, the quantification of preand postoperative total spherical aberration is a closer indication of the real anatomical change obtained by modifying corneal asphericity.
The aim of this article is to describe, in practical terms for the refractive surgeon, the influence of SA on presbyopia and the fundamentals for improving its symptoms during corneal correction with laser by modifying corneal asphericity.
Fundamentals of SA and its relation to presbyopia
In simplified terms, spherical aberration (SA) can be described as a high-order
 aberration caused by an unequal convergence of the central and peripheral rays passing through the refractive surfaces of the eye and striking parallel to the optical axis4. Total SA is defined as the sum of the SA of the anterior and posterior surfaces of the cornea and the lens-induced SA; the total SA will eventually affect the image formed on the retina and therefore, visual quality.
aberration caused by an unequal convergence of the central and peripheral rays passing through the refractive surfaces of the eye and striking parallel to the optical axis4. Total SA is defined as the sum of the SA of the anterior and posterior surfaces of the cornea and the lens-induced SA; the total SA will eventually affect the image formed on the retina and therefore, visual quality.Two main types of SA are described. If in an optical system the peripheral rays from the object focus behind the plane where the central rays focus, it is said that the system has negative spherical aberration (-SA); when it is the other way around, it is said that it has positive spherical aberration (+SA)4.
Well-known examples are: the aberration induced by myopic corneal treatments which make the cornea more oblate, increasing +SA, and hyperopic treatments which make the cornea more prolate, increasing -SA5 (Figure 1).
The relationship between SA and refraction
The interaction between SA and ocular refractive status is not a recent discovery. An attempt had already been made in 1944 to describe this phenomenon6, although it was not always well understood. We currently know that the presence of a spherical aberration in an optical system displaces the best image plane with regard to the plane where the paraxial rays are focused (the paraxial plane), in such a way that the induction of -SA will modify the ocular refractive status, making it more hyperopic; on the contrary, if +SA is induced, there will be myopic displacement.
Data of practical interest for refractive surgery can be obtained from these phenomena, and can be summarised as follows: if we obtain emmetropia in the presence of a certain amount of SA, as the latter decreases, the ocular refractive status (best image plane) will tend towards hyperopia; if this pre-existing SA increases, it will tend towards myopia (Figure 2).
To understand how these optical or refractive phenomena can affect presbyopia, we must first further explain the relationship between SA and pupil diameter,
 as it is one of the major modifying agents that affects SA-induced refractive change (Invest Ophthalmol Vis Sci 2006; 47: E-Abstract 5844). The influence of the pupil is obvious if we take into account that if we decrease the diameter of the pupil, the peripheral rays will gradually disappear until there is only one focus: the central one (very close to the paraxial one). Therefore, if an average eye presents SA, it will be highest with a wide pupil, and will gradually decrease until it practically disappears during pupil miosis, just as it does during physiologically-activated accommodative miosis in near vision7. (Figure 3)
as it is one of the major modifying agents that affects SA-induced refractive change (Invest Ophthalmol Vis Sci 2006; 47: E-Abstract 5844). The influence of the pupil is obvious if we take into account that if we decrease the diameter of the pupil, the peripheral rays will gradually disappear until there is only one focus: the central one (very close to the paraxial one). Therefore, if an average eye presents SA, it will be highest with a wide pupil, and will gradually decrease until it practically disappears during pupil miosis, just as it does during physiologically-activated accommodative miosis in near vision7. (Figure 3)We can thus derive a first refractive aspect that is not yet fully disseminated among ophthalmologists. A patient with emmetropic refraction and significant positive SA, such as can be present after classic myopic lasik treatments, will really have a fluctuating refraction depending on the pupil diameter, so that when the pupil contracts during accommodative miosis, the disappearance of SA will cause a
 hyperopic shift in the refractive state of the eye (Figure 4) that must be compensated by accommodation (accommodative lag), exacerbating presbyopia symptoms, Postoperatively, this is usually identified by the ophthalmologist as an early presbyopia manifestation, when what really occurs is that an increase in +SA causes proportional worsening of symptoms3,8.
hyperopic shift in the refractive state of the eye (Figure 4) that must be compensated by accommodation (accommodative lag), exacerbating presbyopia symptoms, Postoperatively, this is usually identified by the ophthalmologist as an early presbyopia manifestation, when what really occurs is that an increase in +SA causes proportional worsening of symptoms3,8.The contrary is true for negative SA. An emmetropic eye with -SA, such as we can find after total hyperopic ablation, will have myopic refraction during accommodative miosis (Figure 5), improving presbyopia symptoms3,8. Therefore, the presence of a certain degree of -SA can be beneficial for a patient with presbyopia. Presbyopic lasik (also known as "presbylasik") is based on this optical phenomenon, modifying the Q factor which, as we shall see, is ultimately based on the customised modification of the total SA.
Therapeutic approach by customised induction of SA
We can already describe an approach that allows us to treat presbyopic patients with corneal ablations, based on four points in the following order:

1.) Avoid inducing +SA. Even though new aspheric profiles in currently used laser platforms have decreased the amount of induced +SA, especially in moderate to high myopia, if no adequate preventive measures are taken, +SA is still significantly induced.
2.) Reduce pre-existing +SA. The human eye has a slightly positive mean total +SA, of the order of 0.12 µm9,10. This relatively small amount of SA may still induce a hyperopic shift during pupillary miosis (approx. 0.3 D) and must be corrected. This effect will be greater when dealing with higher preexisting +SA3.
3.) Induce -SA when necessary. By using an approach that has already been described2,3, we can induce a certain amount of net -SA to obtain a relative myopic shift during accommodative miosis, creating what has been called "accommodation by pupil miosis", that allows us to further improve the symptoms of presbyopia. Recent theoretical studies have shown that this effect can add approximately 0.7 D to the eye, assuming a wide pupillary range is present (6 to 2 mm)3. However, in order to achieve this, we must first avoid and/or remove all +SA.
4.) Add small amounts of monovision (micro-monovision). A certain amount of monovision may be more efficient and better tolerated in the presence of -SA11. This is true if we take into account that when reducing +SA, micro-monovision offers a complementary and significant addition that would otherwise be insufficient if +SA was present.
Relationship between SA and corneal asphericity (Q factor)
So, how can we reduce +SA and even induce a certain amount of -SA? One way to achieve this is by modifying the corneal asphericity.
Corneal asphericity refers to the difference between the central and peripheral radii of curvature12. This difference is expressed by means of different form factors such as the well known Q factor or eccentricity; its conversion factor is based on the formula (P = Q + 1=1=1�e2 =E�1)7.Tosimplify,wewillexpressit using the Q factor.
There is a close relationship between the Q factor and the induced SA such that as the Q factor becomes more negative, or the lower it is, the more the total SA decreases or becomes negative and vice versa13. The normal human cornea has a Q value of -0.26, corresponding to a certain amount of +SA14,15. In classic myopic laser treatment, the Q factor becomes more positive, inducing +SA15, which is exactly what we have to avoid; this can be achieved by modifying corneal asphericity during laser treatment. An increasing number of laser platforms currently allow the Q factor to be modified at the time of myopic or hyperopic treatment.

How much though do we have to modify this factor, and what are the limits of this modification? This is probably the most sensitive issue pertaining to this technique, as inducing an excessive -SA < -0.4 µm is not only ineffective3, but can also negatively affect the final visual quality16. Decreasing the Q factor to approximately -0.7 at 20o from the centre of the cornea is, in most cases, enough to free an average eye from any amount of significant pre-existing SA3, which in addition to not hindering visual quality, does not worsen presbyopia symptoms, allowing satisfactory near vision without correction in most patients until the age of 45. After this age, if we want to extend the effectiveness of the treatment to as many years as possible, we usually have to induce -SA, and therefore the Q factor must be decreased further than -0.7. This is a more complex field, as the final SA will depend on three major modifiers or preoperative variable factors: pre-existent total SA, Q factor and pupil range. As a rule, we can consider two potential scenarios in which we should not exceed the final target Q value of -1:
a) Patients with scotopic pupil diameter > 6 mm.
b)Patients with lower pre-existing physiological +SA, particularly in those uncommon, albeit possible, cases in which it is already negative.
Tables 1 and 2 show different surgical examples of how the Q target must be adjusted to avoid exceeding -0.4 µm of -SA, depending on the two major modifiers: preoperative total SA (Table 1) and the pre-existing corneal asphericity (Table 2).
Other variables or minor modifiers such as the magnitude of the ablation to be corrected (variation in the corneal radius) are barely clinically significant3. The third major modifier, pupil range, is probably the most important with regard to the decision of whether or not to modify the Q value. A wide pupil range, from 6 mm in meso-scotopic to 2 mm in accommodative miosis, will offer the greatest refractive benefit or accommodation by pupil miosis, thus achieving an extra addition for near vision, derived from the removal of pre-existing +SA and the induction of �SA.
On the other hand, patients with limited pupil ranges or with small pupils will not obtain a significant accomodative benefit from modifying the Q factor. As we have previously mentioned, the total SA practically disappears for pupil diameters smaller than 3 mm. (Figure 3)
Influence of the Q factor on the nomograms
We have mentioned the importance of customized modification of the Q factor in order to correct or induce SA. Nonetheless, this manipulation will give rise to a clinical problem due to the change in final refraction that systematically accompanies this modification hypercorrection in myopic ablations and hypocorrection in hyperopic ablations. For this reason, the nomogram must be customised for each laser platform. This modification is reasonably straightforward in those models that have software indicating the microns of ablation in each treatment, either standard or with modified Q factor. We can thus prevent hyperor hypocorrections by increasing or decreasing the spherical component to be corrected until the final ablation microns of the customised treatment match those of the standard treatment.
Quantifying anatomical results
Quantification of the anatomical results through corneal topography can be difficult to interpret.
Issues such as in which optical area the modification of the Q factor obtained should be assessed, and the variations existing between the different instruments make it advisable to study the results indirectly through measurement of total aberrometry. Thus, the quantification of preand postoperative total spherical aberration is a closer indication of the real anatomical change obtained by modifying corneal asphericity.
CONCLUSION
It would be more accurate to refer to Q factor presbylasik, as presbylasik by customised spherical aberration. In the light of present knowledge, and if there is a wide pupil range, the progressive negativization of total SA may enable an improvement in presbyopia symptoms by customising the Q factor during refractive photoablation, taking into account that there are certain limits to this modification that must be observed in each case so as not to affect the final visual quality.
REFERENCES
- Mrochen M. Hyperprolate corneas for pseudo-presbyopia correction. Cat Refr Surg Today Eur. 2009; 4(1): 28-29.
- Koller T, Seiler T. Four corneal presbyopia corrections: simulations of optical consequences on retinal image quality. J Cataract Refract Surg December. 2006; 32:2118-2123.
- Amigo A, Bonaque S, Lopez-Gil N, Thibos L. Simulated effect of Corneal Asphericity Increase (Q factor) as a Refractive Therapy for Presbyopia. J Refract Surg. 2012;28(6):413-418.
- Atchinson DA, Smith G. Optics of the human eye. Oxford: Butterworth, Heinemann. 2000; 13-16.
- Yoon G, Macrae S, Williams DR, Cox IG. Causes of spherical aberration induced by laser refractive surgery. Cat Refr Surg Today Eur. 2005;31(1):127-135.
- Ta-Hang W. Note on the best focus in the presence of spherical aberration. Proc Phys Soc. 1941;53:157.
- Calossi A. Corneal asphericity and spherical aberration. J Refract Surg. 2007;23(5):505-14.
- Theagarayan B, Radhakrishnan H, Allen PM, Calver RI, Rae SM, O'Leary DJ. The effect of altering spherical aberration on the static accommodative response. Ophthal Physiol Opt. 2009;29: 65-71.
- Khan S, Rocha G. Cataract surgery and optimal spherical aberration: as simple as you think? Can J Ophthalmol. 2008;43:693-701.
- Smith G, Cox MJ, Calver R, Garner LF. The spherical aberration of the crystalline lens of the human eye. Vision Res. 2001;41:235-43.
- Reinstein DZ, Archer TJ, Gobbe M. Aspheric ablation profile for presbyopia corneal treatment using the MEL80 and CRS Master Laser Blended Vision module. J Emmetropia. 2011;2:161-175.
- Lindsay R, Smith G, Atchison D. Descriptors of corneal shape. Optom Vis Sci. 1998;75:156-158.
- Holladay J. Spherical aberration: the next frontier. Cat Refr Surg Today Eur. 2006;6:95-101.
- Navarro R, Santamar�a J, Besc�s J. Accommodationdependent model of the human eye with aspherics. J Opt Soc Am A. 1985;2(8):1273-1281.
- B�hren J, Nagy L, Yoon G, MacRae S, Kohnen T, Huxlin KR. The Effect of the Asphericity of Myopic Laser Ablation Profiles on the Induction of Wavefront Aberrations. Inv Ophthalmol Vis Sc. 2010;51(5): 2805�2812.
- Yamaguchi T, Dogru M, Yamaguchi K, Ono T, Saiki M, Okuyama H, et al. Effect of spherical aberration on visual function under photopic and mesopic conditions after cataract surgery. J Cataract Refract Surg. 2009;35(1):57�63.
| Privaci Policy Ι Contact | COPYRIGHT ® 2012 JOURNAL OF EMMETROPIA. ALL RIGHTS RESERVED |